Fundoplikaciâ – Endoscopic surgery
Opïsanïe éndoskopïçeskoy fwndoplïkacïï
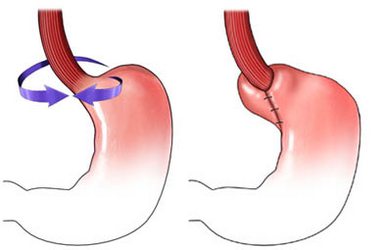
Fundoplikaciâ – surgery on the stomach and esophagus. It is conducted for the treatment of gastroesophageal reflux disease (GERD). GERD is also called acid reflux. It arises, when the acid from the stomach into the esophagus lying. During the procedure, it can be detected by a hiatal hernia. This type of hernia occurs, when part of the stomach penetrating into the chest cavity. This type of hernia increases the chance and severity of GERD.
Reasons for endoscopic fundoplication
The operation is most often performed for the following reasons:
- Eliminate persistent GERD symptoms, that do not pass after taking medicines;
- Reducing heartburn, which helps to reduce the symptoms of asthma;
- Surgery to correct hiatal hernia, disorders that may be responsible for the symptoms of GERD;
- In order to eliminate the source of serious long-term complications as a result of contact with a large amount of acid in the esophagus.
Possible complications of endoscopic fundoplication
If you plan to fundoplication, you need to know about possible complications, which may include:
- Infection;
- Bleeding;
- Difficulty swallowing;
- Resumption of reflux symptoms;
- Limiting the ability to burp or vomit;
- Damage to organs;
- Reaction to anesthesia.
In rare cases, the procedure must be repeated. This may be the case, If there is a new focus of hernia.
Some factors, which can increase the risk of complications:
- Existing heart or lung disease;
- Obesity;
- Smoking;
- Diabetes;
- Previous upper abdominal surgery.
How is the endoscopic fundoplication?
Preparation for the procedure
It can be assigned the following:
- Physical examination;
- Roentgen – analysis, which uses radiation, to take a picture of structures in the body, particularly in bone;
- Endoscopy – using a tube with an attached viewing device (endoscope) to study the internal mucosa of the esophagus and stomach. This may be accomplished biopsy;
- Manometrija – test, to measure the muscular contractions inside the esophagus and its response to swallowing.
On the eve of the operation:
- Consult your doctor about the drugs taken. A week before surgery you may be asked to stop taking some medicines:
- Anti-inflammatory drugs (eg, aspirin);
- Blood thinners, such as warfarin;
- Clopidogrel;
- We need to organize a trip to the procedure and back. Besides, take care of the home care;
- On the eve of the operation in the evening you can eat a light meal. Do not eat or drink anything after midnight.
Anesthesia
Used general anesthesia, which blocks any pain and the patient support in a sleep state during operation.
Description endoscopic fundoplication procedure
The doctor inserts an endoscope – tube with a light source and a camera on the end, through the mouth and throat into the esophagus. When the endoscope reaches the upper part of the stomach, Your doctor can perform one of the procedures, which reduce the emission of gastric acid into the esophagus.
How long will the endoscopic fundoplication?
Less than an hour.
Endoscopic fundoplication – Will it hurt?
During recovery, you will have discomfort. Doctor will prescribe painkillers, to reduce discomfort.
The average hospital stay
2-3 day. Perhaps less, if the recovery is fast.
Care after endoscopic fundoplication
- Start walking with assistance the day after surgery;
- You can start eating, starting with liquid food. You will gradually be able to switch to solid food;
- After a successful fundoplication, you no longer need to take medicines for GERD;
- Be sure to follow your doctor's instructions.
Recovery will take about six weeks.
Contact your doctor after endoscopic fundoplication
After returning home, you need to see a doctor, If the following symptoms:
- Signs of infection, including fever and chills;
- Nausea and / or vomiting, which do not disappear after taking the prescribed medicines, and persist for more than two days after discharge from the hospital;
- Increased swelling or pain in the abdomen;
- Difficulty swallowing;
- Pain, which does not pass after taking pain medication appointed;
- Pain, burning, frequent urination or persistent blood in the urine;
- Cough, shortness of breath or chest pain;
- Other painful symptoms.
