Transplantation of pancreatic islets – Transplanting islet cell
Description islet cell transplant
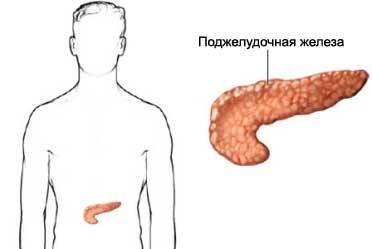
Islet cells (islet cells) – cells of the pancreas, produce insulin. Transplantation of pancreatic islets – islet transplantation donor cells from another person. At this point, the procedure is being studied as a treatment of chronic pancreatitis and diabetes type 1.
Reasons for islet cell transplantation
Cells of pancreatic islets consist of alpha- and beta-cells. Diabetes 1 such as developing, when the beta cells of the pancreas are destroyed by the immune system of the organism's own. Without these cells the body can not produce insulin (needed to break down glucose). As a result, patients with diabetes 1 type need daily injections of insulin.
Although the procedure of transplantation of pancreatic islets is at the stage of the experiment and study, already it is seen that the transplanted islet cells can produce insulin. After one or two injections of islet cells, some patients may stop taking insulin for some time.
Possible complications of transplantation of pancreatic islets
If you plan to transplant islet cell, you need to know about possible complications, which may include:
- The toxicity of immunosuppressive drugs;
- Damage to the liver and pancreas;
- Problems with cholesterol;
- Sensitization – the recipient cells may form antibodies to re-islet cell transplantation;
- Nausea, vomiting, abdominal pain;
- Bleeding;
- Infection;
- Blood clots;
- Deterioration of renal function;
- The deterioration in the presence of high blood pressure;
Factors, that may increase the risk of complications:
- Smoking;
- Kidney disease;
- Blood clotting.
How is the transplantation of pancreatic islets?
Preparation for the procedure
Doctor will prescribe blood tests and a physical exam. Conduct tests, to assess the extent and severity of diabetic complications and possible kidney damage. The donor must also be carefully examined for compliance with blood and serogroup.
Anesthesia
It can be used topically or general anesthesia. Local anesthesia numb the area operation. When using general anesthesia you sleep.
Procedure transplantation of pancreatic islets
Before surgery, islet cells are taken from a donor pancreas. Usually, these cells to be used in the next 24 hours.
The abdominal incision is made small. Catheter (a small plastic tube) inserted through an incision in the large blood vessels of the liver. To find the correct position of the catheter will be used US. Then the catheter is inserted through the islet cells. The cells are moved through the vein to the liver, and then begin to produce insulin.
Immediately after transplantation of islet cell
It is important to maintain normal blood glucose levels. High levels of glucose can cause damage to the new islet cells. During the first few days after transplant, through the IV will inject insulin. This will help to maintain normal blood glucose levels.
Your immune system begins to attack the transplanted cells. To prevent this, you need to take medication, that suppress the immune system.
Such drugs, suppress the immune system, usually, must be taken for life. This will prevent rejection.
How long will the islet cell transplant?
About an hour.
Transplanting islet cell – Will it hurt?
The introduction of local anesthetic can cause a burning sensation. Anesthesia will prevent pain during the procedure. After the procedure, some patients experience pain for a few days. If you have discomfort, the doctor will give painkillers.
The average time of hospital stay
3-4 day.
Care after transplantation of pancreatic islets
- Keep the incision clean;
- Follow your doctor's instructions for the care of the operational seam;
- Frequently check blood glucose levels. Follow your doctor's instructions;
- Control your blood sugar using insulin.
The doctor may repeat several times a transplant, to introduce more islet cells.
Communication with the doctor after the transplantation of pancreatic islets
After discharge from the hospital need to see a doctor, If the following symptoms:
- Signs of infection, including fever and chills;
- Redness, edema, increased pain, bleeding or discharge from the incision;
- Cough, breathlessness, chest pain, severe nausea or vomiting;
- High or low blood glucose levels.
