Cytological diagnosis of tumors of male genital organs
Testicular tumors
Testicular tumors up 2 % of all malignancies in men. In children, these tumors occur much less frequently, primarily during the first three years of life. Men tumor eggs develop at any age, but most often between 20 and 45 years.
With the same frequency affects both testicles, although some authors noted more frequent lesion of the right testicle. Maybe, this is due to the most common right-sided cryptorchidism. The simultaneous loss of both testicles is rare.
The bulk of testicular tumors account for malignant neoplasms, benign tumors are very rare.
Testicular tumors, usually, primary, except for his defeat in leukemia and retikulosarkome. However, in these cases, the affected testicle is often the first place.
Metastasis of other tumors occur rarely in the testis.
According to histological classification, the following types of testicular tumors.
Germ cell tumors
Tumors of the histological type
- Seminoma
- Spermatocytes seminoma
- Эmbrionalynыy cancer
- Yolk sac tumor (infantile embryonal carcinoma type; opuholʹ éntodermalʹnogo sinuses)
- Poliembrioma
- Xoriokarцinoma
- Teratoma: and) mature; to) immature; in) with malignant transformation
Tumors of more than one histological type
- Embryonal carcinoma and teratoma (teratocarcinomas)
- Choriocarcinoma and other
- Other combinations
Stromal tumor sexual roller
Well differentiated form
- The tumors of the testis glandulotsitov (interstitial eidokrinotsitov, or Leydig cells)
- Tumors of the supporting cells of the convoluted seminiferous tubules (sustentocitov, or Sertoli cells)
- Folliculoma
Mixed form
Do not fully differentiated form
Tumors and tumor-like lesions, containing germinal cells and stromal elements of the reproductive platen
Gonadoblastoma
Other
Other tumors
Tumors of lymphatic and hematopoietic tissue
Secondary (metastatic) tumor
Tumors straight seminiferous tubules, rete testis, epididymis, spermatic cord, capsules, support structures and rudimentary formations
Adenomatoidnaya tumor
Mesothelioma
Adenoma
Cancer
Melanotic neuroectodermal tumor
Brenner tumor
Soft tissue tumors
Unclassified tumors
Tumor-like lesions
Germ cell tumors
Germ cell tumors (of the germ cells) account for about 97 % all testicular neoplasms. By cell composition may be homogeneous (seminoma, эmbrionalynыy cancer, xoriokarцinoma) and patchy (teratomatous tumor).
Seminoma - dysgerminomas – Spermatoblastoma
Seminoma (disgerminoma, spermato- blastoma et al.) - The most common tumor of germinal. Often developing testicular teratoma at the same time. Most often seen in the right testicle, but possibly bilateral disease. There are the typical, and anaplastic seminoma Spermatocytic.
Typical seminoma grows in the form of single or multiple nodes unencapsulated rounded shape. Metastasizes first to the nearest lymph nodes, and then the internal organs. Microscopically the tumor is the same type of round or oval cells of large or medium-sized. The cell nuclei large, with delicate chromatin structure, contains 1-2 nucleoli, often arranged eccentrically. Many pieces of division.
The cytoplasm of cells in stained basophilic due to the large amount of glycogen, vacuolized.
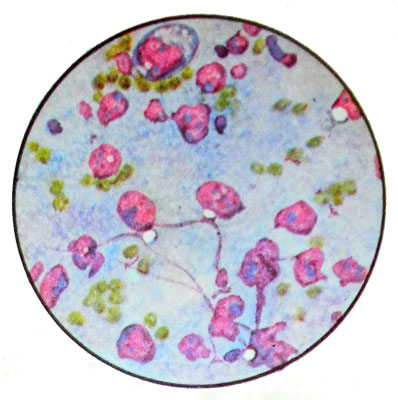
In almost all cases, the drugs are present lymphoid elements, They may also occur fibroblasts, gistiocitы, epithelial cells and cell type Pirogov-Langhans. In the presence of areas of necrosis and tumor above elements must be distinguished from tuberculosis.
Anaplastic seminoma appearance is not different from the classic. Microscopic cells characterized by a pronounced polymorphism, their different sizes, up to giant. Kernels large, irregular shape, with a rather coarse structure of chromatin and nucleoli. Multinucleated cells found.
Spermatocytic seminoma (spermatocitoma) is less than 5 % All seminomas. Observed in men over 40 years. Grossly the tumor yellow, It has a spongy structure. Hemorrhage and necrosis are absent in it.
Microscopically, there are three types of tumor cells:
- medium sized with rounded, a relatively small nucleus and cytoplasm wide rim;
- small limfotsitopodobnye;
- large single, bi- or multi-core.
This seminoma Spermatocytic named because of the similarity of the nuclei of tumor cells with mature forms of spermatogenesis. In mikroskopicheskom issledovanii spermatotsitnuyu seminomu necessary differentsirovaty with retikulosarkomoy yaichka.
Эmbrionalynыy cancer
The tumor develops from the undifferentiated cell types of somatic and extraembryonic. It is soft consistency, mottled on the cut thanks to the numerous areas of necrosis.
The most common type of somatic embryonal carcinoma. Microscopically, it is characterized by a pronounced polymorphism with a predominance of large cells. Many giant one- and multi-dividing cells, resembling epithelial cells, with fuzzy boundaries, large vesicular, hyperchromatic nuclei, containing nucleoli. Basophilic cytoplasm. Cells are arranged individually or in the form of glandular and papillary structures.
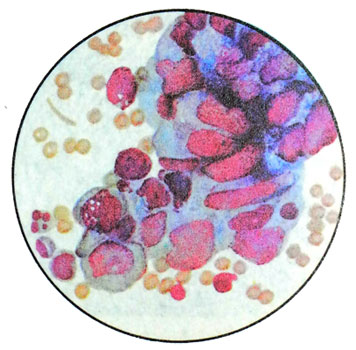
This type of cancer can be combined with seminoma.
Yolk sac tumor
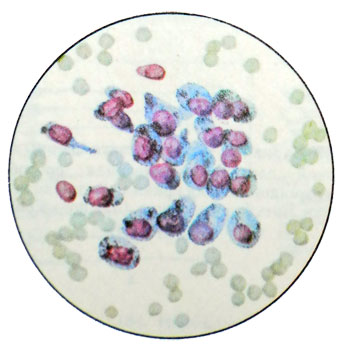
Usually occurs in children, rarely can occur in adults of both sexes. Microscopic examination revealed a cube-shaped cells with large nucleus, arranged eccentrically due to the presence of large cytoplasmic vacuoles, pushes the core to the shell. Loosely arranged cells, in the form of iron-looped structures. There may be tumor cells of mesenchymal nature.
The tumor can be detected punctate glomerulopodobnye calf, representing small cysts, which protrudes into the lumen of the papilla, equipped with a capillary. Papilla and wall cysts are lined with vacuolated cells cube-shaped and flattened cells endoteliopodobnymi. The combination of morphological features of the yolk sac tumor and embryonal carcinoma. Sometimes, punctate tumor found in the embryoid bodies, consisting of the elements, characteristic of the early stages of embryo development. With a significant amount of swelling embryoid bodies treated as poliembriomu (a kind of embryonic cancer).
Xoriokarцinoma (horionэpitelioma)
Morphologically similar to horiokartsinomoy yaichnika.
Teratoma
In the formation of teratomas participate derivatives of all germ layers. Among testicular tumors occur relatively frequently (7z in all cases). Develop at any age. The morphological features distinguish the mature, immature teratoma and malignancy.
Mature teratoma testicle rarely observed. Consisting mostly of mature tissues of different origin (glands, cyst, cavity, lined with intestinal-type epithelium and squamous epithelium, Liver tissue sections, thyroid and pancreas, Nervous, cartilaginous, bone).
Despite the maturity of these tissues, mature teratoma has signs of cancer. In its metastases are found mature and immature elements. According to the morphological structure of the tumor metastasis is significantly different from the primary tumor and often resemble embryonal carcinoma or choriocarcinoma. A dermoid cyst develops in a testicle is significantly less, than in the ovary. Mature teratoma testicle may occur along with seminoma.
Immature teratoma. Unlike mature teratoma tumor consists mainly of immature tissues, like tissues of the embryo. There may also lymphoid, cartilaginous, connective tissue cells, neurogenic epithelium etc..
Can meet and lots of mature tissue. The tumor is often combined with embryonic carcinoma.
Malignancy teratoma It is extremely rare. It is characterized by severe malignant transformation of epithelial cells or cells of mesenchymal origin. In the first case, the cancer develops, Second - sarcoma.
Sex cord stromal tumors
Leydigoma
Leydigoma - Interstitial tumor, developing from glandulotsitov (interstitial endocrinocytes, or Leydig cells), It has a view of a brown, clearly delineated from the surrounding tissue. It occurs at any age. Boys leydigoma cause premature puberty, men are often seen feminization. The tumor is benign, but sometimes metastasizes.
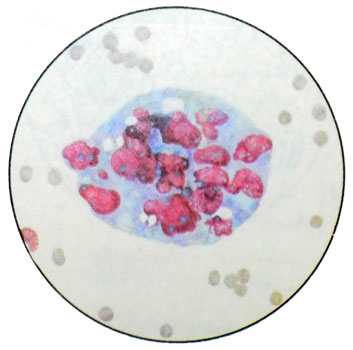
Microscopic examination revealed cells of various sizes and shapes, with, as normal glandulotsity, a different degree of maturity and are different in phase functional activity. The most common cells of medium size, round, oval or polygonal shape with enlarged, eccentrically located nucleus, containing nucleoli. Basophilic vacuolated cytoplasm containing brown pigment, lipids and proteins occasionally krïstalloïdı Reyneke. In stained preparations crystalloid Reynard have the form of colorless elongated rods with rounded or be chopped off ends. Even normally are not found in all the interstitial endocrine cells.
The punctate tumor You can find a variety of cells with a predominance of the two major- and multi-forms. The native samples detected in the cytoplasm lipid-containing vacuoles. There may be an elongated spindle-shaped cells, Alopecia frequently ranging around the vessels or in the form of strands. In a typical hyperplasia glandulotsitov, such as cryptorchidism, You can observe a similar picture. However, in the latter case, do not appear visible to the eye tumor and nodes are retained testicle interstitial tubules, which can be determined only by histological examination.
Sertolioma
The tumor develops from the supporting cells of the convoluted seminiferous tubules (sustentocitov, Sertoli cells). It refers to the immature tumors, histological similar tekomoy. The spread of the tumor outside the testis and metastasis are rare. Microscopically detected three types of cells: 1
- a cylindrical shape with an oval nucleus, having nucleolus, and by a narrow rim of cytoplasm with lipoid inclusions;
- cubical, somewhat smaller, arranged as nests and cords;
- light, glandulotsity and features resembling strands.
Tumors and tumor-like lesions, containing germinal cells and stromal elements of the reproductive platen
There are at gonadal dysgenesis and cryptorchidism.
Gonadoblastoma
Tumors develop at any age. IN 1/3 cases there is bilateral involvement of the testes. Often marked hormonal disorders, which are clinically manifested in the form of feminization or virilization.
The tumor is characterized by two components:
- germinal cells;
- stromal cells sexual roller.
Germinal cells microscopically detected type of cell seminoma with frequent mitosis and cell type of immature support cells of the convoluted seminiferous tubules or granulosa, and sometimes cell, Similar to glandulotsitami (interstitial endocrinocytes). The punctate frequent hyaline or acervulus.
Metastasize usually only germinal component of tumor. Most often, patients have a female phenotype gonadoblastomoy. In the absence of chromosomal abnormalities talk about atypical gonadoblastome.
Tumors straight seminiferous tubules, rete testis, epididymis, spermatic cord and seminal vesicles
Neoplasms of this localization are rare. Usually it is an adenoma and adenocarcinoma, with the cubic and flattened cylindrical cells form papillary proliferation, sometimes resembling tsistadenopapillomu.
When adenocarcinoma observed hyperchromia nuclei and their piling in papillary structures.
Tumors of the epididymis and egg shells, spermatic cord may be epithelial and non-epithelial, benign and malignant.
Epithelial tumors localized in the epididymis, non-epithelial - In the spermatic cord and testicle membranes. Microscopically characterized by the presence of cells of cubic shape or flattened, sometimes epithelioid type. They are located in the form of strands or papillary formations. There are cells with the growth of muscle fibers neischerchennyh, whereby the tumor resembles leiomyoma. Can detect areas with lymphoid infiltration and necrotic foci.
The spermatic cord may develop tumors, typical of soft tissues - lipoma, fiʙroma, angioma, neurofibroma, etc.. Occasionally in the elderly may cause testicular mesothelioma. Microscopic examination revealed the same type of cells are round or oval in the form of papillary excrescences and psammous cells.
Of the various types of sarcomas often observed juvenile rhabdomyosarcoma spermatic cord, that extends to the egg. May develop undifferentiated sarcoma of the stellate mesenchymal cells.
For tumors of hematopoietic tissues are:
- multiple myeloma (myeloma);
- lymphosarcoma, etc..
Tumors of the penis
These tumors develop from the skin of the penis and its appendages, corpus cavernosum and urethra. Cancer of the penis It is often. Usually it is preceded by proliferative processes, leukoplakia, kondiloma, papilloma.
By precancerous conditions also include Keira erythroplasia and Bowen's disease. From the morphological variants of cancer most often develops squamous.
For tumors of the cavernous bodies are fiʙroma, Angioma and their malignant counterparts.
Tumors of the prostate
The prostate gland can develop premalignant processes, benign and malignant tumors.
Precancerous diseases of the prostate
By precancerous diseases include nodular hyperplasia. In the prostate, mainly in its middle lobe, produced multiple nodes, which leads to an increase in whole body. It occurs in 55-60 years of age. Microscopically punctate found in the same type of high prismatic epithelium cells with hyperchromatic nuclei in the basal cells and pale cytoplasm, containing grain, and in the apical part of the fat droplets. Located epithelium a papillary formations. Besides, It can be detected in a punctate metaplazirovanny epithelium, especially after treatment sinestrol, and leukocyte accumulation, macrophages and amyloid corpuscles.
Benign prostatic tumors
Adenoma. It grows as a single unit, microscopic similar nodulyarnoy giperplaziey and svetlokletochnoy adenokartsinomoy. It is found in the age of 40 years.
Leyomyoma. Microscopically no different from those of tumors at other sites. It occurs in people 40-50 years.
Malignant tumors of the prostate gland
Prostate Cancer develops in people older 50 years, with the age of its frequency increases. During slow cancer, Early diagnosis is very difficult. Metastasize not only the internal organs, but also in bone, particularly common in the pelvis and vertebrae. Histologically prostate cancer characterized by considerable polymorphism even within the same tumor.
Razlichayutsleduyuschie prostatic cancers:
- Adenocarcinoma;
- Temnokletochnыy tubulyarnыy cancer;
- Svetlokletochnыy tubuloalyveolyarnыy cancer;
- Slizyeprodutsiruyushaya adenocarcinoma;
- Kribroznыy cancer;
- Solidly-trabecular transitional cell (similar to that of bladder cancer);
- Ploskokletochnыy cancer (rarely);
- Nedifferentsirovannыy cancer.
