Anemia, associated with disruption of the structure of globin chains
Anemia, associated with disruption of the structure of globin chains, hemoglobinopathies, or - a group of diseases, due to the replacement of one or more amino acids in the chain globin, the absence of the chain, or its extension.
The clinical picture of hemoglobinopathies It depends on the location of substitution. Haemoglobin disorders can manifest anemia, not make any changes in the blood or determining increase in hemoglobin and red blood cells.
The first description of hemoglobin restructured refers to 1949 city, when it was discovered, that the sickle cell hemoglobin, moving electrophoresis in alkaline medium with a velocity, at, than adult hemoglobin.
IN 1956 g using the method of peptide maps installed, hemoglobin, detected at sickle cell anemia and called hemoglobin S, It differs from healthy human hemoglobin A change only a single amino acid chain β-. Normally, in the sixth position of β-chain N-terminal is glutamic acid, and with hemoglobinopathies S - amino acid valine. It differs in charge of the glutamic acid, hemoglobin therefore moves in an electric field at a lower speed.
Most hemoglobinopathies not provide any clinical manifestations in the heterozygous, either in the homozygous state. It is observed in those cases, When amino acid substitutions do not destroy the tertiary or quaternary structure of hemoglobin and hemoglobin basic functions are stored. Part of the haemoglobinopathies gives clinical manifestations in homozygote form or in combination with Thalassemia. Sometimes the clinical signs of the disease are detected from heterozygous carriers of the abnormal gene, if you have a group of unstable abnormal haemoglobins. When these gemoglobinopatijah replacement for the most functionally important amino acids. These amino acids are involved in fixing the heme to globinu, coupling circuits globin gene among themselves.
Serpovidnokletochnaya anemia, haemoglobinopathies, S, (C) widely disseminated in various African countries. Among the most common forms of haemoglobinopathies include haemoglobinopathies (E), Danswer.Replacement of the amino acid β-chain occurs much more frequently, than α-chains.
For the identification of abnormal hemoglobin must first establish its presence in a patient. Hemoglobin S and stable gemoglobiny identified during electrophoresis on acetatcelljuloznoj film, paper. However, electrophoretic study provides an opportunity to identify only 1/3 part of abnormal haemoglobins. When anemia, associated with the violation of the structure of globin gene circuits, diagnosis of hemoglobinopathy only when it detects signs of instability of hemoglobin, often, in the absence of changes in electrophoretic mobility.
After identifying the signs of abnormal hemoglobin becomes necessary to his Office one way or another (electrophoresis, thermal denaturation, chromatography) from normal hemoglobin (A), clarifying the chain, which replacement takes place (methods of gidrolizacii chains, Enduro or chromatographic separation of their).
The next step is to tripsinovyj hydrolysis of abnormal circuits, obtaining peptide maps to clarify peptide, in which there is an anomaly, study of amino acid composition of pathological peptide, If necessary, study the order of amino acids in a peptide.
In the designation of hemoglobin in addition to its name provides the chain, which replacement takes place, the number of amino acids in the chain (starting with n end), title amino acids, that is on this site, as well as the name of amino acids, that was supposed to be in this section. For Example, Hb Eα2b226Glu → shaft means, What we are talking about the haemoglobinopathies (E), where the substitution takes place 26-th amino acid β-chains-glutamic acid to valine.
Anemia, due to accumulation of hemoglobin, modifying structure in hypoxia
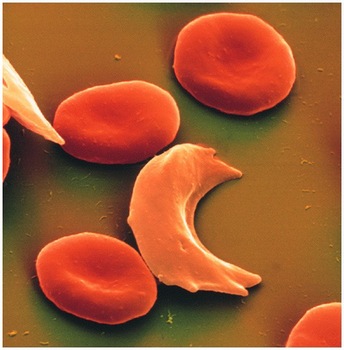
The most frequent abnormality of hemoglobin structure is gemoglobinopatija Sα2b26Glu → shaft. In the case of gomozigotnogo talk about sickle cell anemia, geterozigotnogo is about sickle cell abnormalities.
Drepanocytemia distributed in African countries (Angola, Mozambique, Congo, Liberia, Algeria, Tunisia, etc.). This disease is often found in India, on the island of Ceylon, in Turkey, Iran, Iraq, in Cuba.
The phenomenon of serpovidnosti is a consequence of reduced solubility of hemoglobin, giving oxygen, compared with hemoglobin A. Hemoglobin A, deprived of oxygen, soluble in half, than hemoglobin A, sated with oxygen. Solubility of haemoglobin S when oxygen decreases 100 time. This leads to the formation of the gel. By microscopy detected crystals size 1,5 m, reminding under the form sickle-shaped red blood cells. Crystals, growing up in the same direction, called taktoidami. They disappear when you attach to hemoglobin oxygen. It can be assumed, that the replacement of the glutamic acid in the sixth position in the valine leads to increased a haemoglobin molecules on the other in cases, When a molecule of hemoglobin is not attached oxygen. This and ensures low solubility of the molecule. Presence in the erythrocytes of haemoglobins (C), Danswer, OArab increases the serpovidnosti phenomenon, whereas the presence of hemoglobin (p) in a large number reduces the degree of erythrocyte serpovidnosti.
Homozygous form of haemoglobinopathies, S (drepanocytemia)
Clinically characterized by moderate anemia normohromnoj, thrombosis, the peculiar views of patients. The first manifestations of the disease occur only a few months after the birth of a child, Since fetal hemoglobin, the principal at birth, does not contain abnormal β-chains and not broken. Besides, high level of fetal hemoglobin in young children after appearing pathologic chain reduces the phenomenon of serpovidnosti due to the increased affinity for oxygen.
The most common symptom of sickle cell anemia in early childhood is the defeat of bones and joints.
In connection with the pulmonary vascular thrombosis in children often observed heart light. This process can be accompanied by increased body temperature to high digits, the increase in the number of cells. May develop kidney infarction.
Sometimes during times of increased process in joints or in the lungs of children develop severe hemolytic crises with symptoms of intravascular hemolysis with black urine, the sharp decline in the level of hemoglobin, high fever. In later life to these phenomena often joins the sharp pain in the abdomen, tromboticheskimi-related complications of the disease.
Vitreous hemorrhage and retinal detachment are often the cause of blindness.
Damage to the nervous system may also be due to vascular thrombosis, feeding the various parts of the brain.
In early childhood the spleen enlarged, Thereafter it decreases, and after 5 years of splenomegaly was observed rarely. It is associated with a characteristic symptom of sickle cell anaemia — autosplenjektomiej, caused by fibrosis of the spleen as a result of frequent heart attacks. The liver most often increased.
In adults, suffering from sickle cell anaemia, Sometimes there is priapism, associated, most likely, with the stagnation of sickle cell of erythrocytes in the cavernous bodies, what, in turn, increases hypoxia and sickle cell formation of erythrocytes.
In the study of blood out of focus is found expressed normochromal anemia: hemoglobin 3.72-4.96 mmol/l (60- 80 g / l). In a colored smear can sometimes be identified sickle-shaped red blood cells, However, more characteristic of the presence of Basophilic punktacii erythrocytes, mishenevidnosti. Camber can be detected using samples with sodium metabisul'fatom or by means of a harness at the base of the thumb.
The content of reticulocytes, the number of bone marrow jeritrokariocitov and indirect bilirubin level increased, ESR is most often within normal limits, as sickle-shaped red blood cells settle more slowly, than normal.
Perhaps the presence of sequestration crises, where a large part of erythrocytes disappears in the internal organs. This can lead to the development of collapse, for breeding from which require a quick blood transfusion.
Described aplasticheskie crises, in which expressed anemia, leukopenia, disappearing reticulocyte. They often occur after severe viral infections.
The majority of patients with sickle cell disease die in early childhood. Very high mortality among pregnant women, suffering from sickle cell anaemia. According to some reports, maternal mortality in sickle cell aplazii is 6 %.
Geterozigotnaja form of haemoglobinopathies, S (sickle cell, the anomaly)
In this form of hemoglobinopathy patients sometimes are unaware of their disease, they have normal hemoglobin, satisfactory condition. The only symptom of disease in some patients is hematuria, associated with small infarctions of kidney vessels. The content of an abnormal hemoglobin in erythrocytes of patients with heterozygous hemoglobinopathy form small, clinical manifestations of the disease are observed only during hypoxia, in the case of severe pneumonia, during anesthesia, When flying on razgermetizirovannom plane.
Thromboembolic manifestations can occur in any body, the defeat which occurs with sickle cell anemia. The phenomenon of serpovidnosti is detected in patients when using metabisul'fatnoj samples. When hemoglobin electrophoresis detected two large factions — A hemoglobin and hemoglobin S.
The combination of heterozygous hemoglobinopathy form S (sickle cell disease) with β-Thalassemia.
Occurs frequently, It flows much softer, than homozygous β-Thalassemia and homozygous gemoglobinopatija S.
It is characterized by a significant increase in spleen, pronounced gipohromiej erythrocytes, a large degree of mishenevidnosti. Thromboembolic complications are much less, than in sickle cell anemia. There may be bouts of pain in the joints, stomach. Lag behind in physical development. Characterized by a significant increase in the level of fetal hemoglobin. If there is no A hemoglobin electrophoresis, and hemoglobin S can be almost the only haemoglobin. When β-Thalassemia in addition to Hb S, A2 and fetal haemoglobin is detected by A.
High hemoglobin F serpovidnosti phenomenon is expressed out of focus.
Anemia, due to accumulation of stable abnormal haemoglobins
The most common forms of this anemia are haemoglobinopathies (C), Danswer and E.
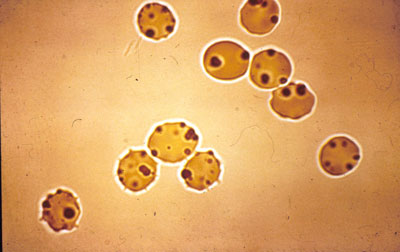
All of these types of haemoglobinopathies in geterozigotnom condition and with their combination with each other or with Thalassemia don't give clinical manifestations. When homozygous haemoglobinopathies with out of focus is found expressed hemolytic anemia with increased spleen and diarrheal phenomena. In biopsy identifies mishenevidnye erythrocytes. With the haemoglobinopathies (D)answer appears in homozygote form extremely rare, and with the haemoglobinopathies E in homozygote form detected out of focus expressed by hemolytic anemia, a slight increase in spleen. A combination of all three types of haemoglobinopathies with Thalassemia causes significantly more severe clinical picture and pronounced increase in spleen.
All three types of hemoglobin are characterized by the replacement of the β-chain. In hemoglobin C 6-e link glutamic acid is replaced by lysine, in hemoglobin E 26-e link glutamic acid is on lysine, in hemoglobin (D)answer 121-(e) link glutamic acid — glutamine.
Mobility of hemoglobin Danswer corresponds to the hemoglobin S mobility, But unlike haemoglobinopathies S haemoglobinopathies (D)answer are normal tests on the solubility and Camber. Mobility of hemoglobin E same, as mobility and hemoglobin A2, but the amount of hemoglobin A2 never such a, as with the haemoglobinopathies (E).
The disease occurs in West Africa, Turkey, Iran, India (Punjab).
Gemoglobinopatija (E) found in India, Cambodia, Burma, Indonesia.
Anemia, due to the unstable accumulation of abnormal haemoglobins
Under unstable gemoglobinami understand these abnormal gemoglobiny, that due to the volatility of molecules precipitate in erythrocytes, that leads to the development of hemolytic anemia in heterozygous carriers of the abnormal gene.
Etiology and pathogenesis
IN 1952 g. Cathie described child with congenital hemolytic anemia, which after Splenectomy in all erythrocytes found Taurus Gejnca. Only after 18 years, it was found, that the cause of these abnormal hemoglobin faction was a Taurus. Initially, this group of diseases called congenital hemolytic anemia with Gejnca cells.
The first unstable hemoglobin structure was installed HbZurich, discovered in 1962 g. two patients, survivors of acute hemolytic crisis after taking sulfanamides.
Research it was found, that part of hemoglobin in patients with cells Gejnca easily precipitates when heated. IN 1969 g. It was suggested that a new name for this group of diseases is hemolytic anemia, due to accumulation of volatile haemoglobins.
This type of anemia is inherited by atheroma. The instability of the molecule of hemoglobin is found in those cases, When the substitution of amino acids related to the linkage with the globin gene haemom, connection α- and β-globin gene circuits between them, as well as when there is substitution of amino acids, falling into a spiral of hemoglobin, amino acid prolinom, which is due to the peculiar structure cannot be part of a spiral.
The instability of the haemoglobin molecules detected in cases, When the plot molecules globin gene, to which adjoins a gem, in the so-called gemovom Pocket, nonpolar amino acid (glycine, valine, alanine, etc.) replaced by polar (glutamine, aspartic, etc.). In this case, the gemovyj Pocket penetrates a water molecule, violates the stability of hemoglobin molecules.
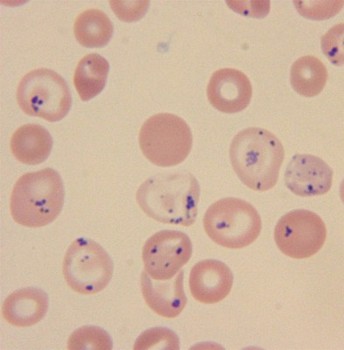
Instability of hemoglobin It may also be due to deleciej one or more amino acids or elongation subunits. This leads to deformation of molecules of hemoglobin and disrupt its stability. As a result, some forms of haemoglobinopathies in erythrocytes appear multiple calf-inclusion, due to precipitation in the sludge of unstable hemoglobin. In other cases, are found in the erythrocytes of sporadic calf Gejnca, constituting or hemoglobin, devoid of heme, or precipitate isolated circuits globin gene.
Clinical manifestations
Clinical symptoms of anemia are varied and depend on the localization of amino acid substitution.
Some patients have hemoglobin normal, among others it is lowered to 2.48-3.72 mmol/l (40-60 G / l). In the case of a heavy course of the disease, or at an average severity of hemolytic anemia clinical manifestations are observed already in childhood. Degree of zheltushnosti, as well as the degree of anemia, depends on the nature of amino acid substitution and sometimes different: some patients skin coloring and skler normal, other marks constant or periodic expressed zheltushnost'. In most patients the spleen enlarged, However, some forms of haemoglobinopathies remains normal. Perhaps enlarged liver. This anemia is often complicated by cholelithiasis. Modify the skeleton can be the same, as in microspherocytosis, in light forms of anemia are they missing.
Laboratory findings
When carriers unstable haemoglobins is detected anemia varying degrees of symptoms, often normochromic, sometimes anaemia, in connection with part of hemoglobin in sediment, especially in those cases, When heme from globin gene otshheplen, or when the precipitate consists of separate circuits. Detected mishenevidnost' erythrocytes, anisocytosis, polihromaziya. Content of reticulocytes always promoted. Notes of red bone marrow germ irritation.
Blood and clinical manifestations of haemoglobinopathies depend only on the character of amino acid substitution. One and the same gemoglobinopatija in patients, non-relatives is an abnormal hemoglobin carriers gives similar clinical manifestations. So, When Biba gemoglobinopatijah, Savannah, Casper, Volga observed clinic severe hemolytic anemia, When gemoglobinopatijah Tacoma, Belfast, Casper, Moscow has minimal clinical manifestations. When part of the haemoglobinopathies is changed to oxygen affinity.
Most gemoglbinopatij with high hemoglobin oxygen affinity is characterized by amino acid substitution in contacts between α- and β-chains (a1b2-contacts). Increased affinity for oxygen may also be associated with changes in amino acids, 2.3 linking related-diphosphoglycerate substances, required for normal impact haemoglobin oxygen tissues. At gemoglobinopatijah, associated with an increased affinity for oxygen, as a result of tissue hypoxia can occur eritrotsitoz, rather than anaemia. Where, When affinity to oxygen is lowered, anemia may occur, due to no increased hemolysis, and giperoksiej. In these cases, it is not the nature of the hemolytic, and associated with a reduction in the level of erythropoietin.
Haemoglobinopathies Diagnostics
Haemoglobinopathies Diagnostics, due to the unstable accumulation of abnormal globinov, It based on the, that when exposed to blood of various oxidizing agents, for example bright blue krezilovogo, some forms of unstable hemoglobin denaturation and subjected to precipitate in the form of small multiple inclusions.
The same inclusion are detected with the haemoglobinopathies (H), Takosha, Moscow. This coloration is typically used for the determination of reticulocytes. For clearly identifying inclusions need more incubation 2 no.
In some patients at colouring as oxidizing, and neokisljajushhimi dyes (eg, Crystal Violet) in erythrocytes identified single large calf Gejnca, arranged eccentrically. Most often they are observed in patients, undergoing splenjektomiju.
Method research of termolabil'nosti hemoglobin is he that, that in the midst of heated to 55 ° C at pH 7,4 in 0,15 M fosfatnom buffer normally via 1 h precipitates on average about 13 % Hemoglobin, in the presence of unstable hemoglobin is more 25 %.
Express-method for detecting unstable hemoglobin, It is as follows. Gemolizat blood is placed in 17 % isopropyl alcohol in TRIS-buffer and intubated with a temperature 37 ° C. In the presence of unstable hemoglobin sediment falls through 5-15 min, While normally it appears only after 30-40 min.
Reagents: 17% solution of isopropyl- pilovogo alcohol 0,1 M buffer solution, TRIS-hydrochloric acid (pH 7,4). The long-term solution may be stored in an air-tight container.
Method. Gemolizat, contains approximately 6,21 mmol / l (100 g / l) Hemoglobin, is made of triple-washed izotoniceski solution of sodium chloride of erythrocytes with added 1-1 5, the volume of distilled water. Erythrocytes shaking gemolizirujutsja, lipids are extracted half the volume of carbon tetrachloride with shaking during 2 m. After centrifugation for 10 minutes at 3000 RPM separates the top layer for research.
Isopropyl alcohol is 2 ml 2 test tubes, closed traffic. The tubes were heated at a temperature of 37 ° C in a water bath. In one of the tubes is poured 0,2 ml gemolizata, obtained from erythrocytes of the patient, in another 0,2 ml gemolizata, obtained from the donor's red blood cells. In the presence of unstable hemoglobin sediment falls through 5-15 min. Possible and erroneous results. If inaccurate, higher concentrations of alcohol, higher temperatures when heated tubes, more acidic pH normal hemoglobin may fall in previously 30 m. At high concentration of methemoglobin sediment may occur at the expense of lesser resistance methemoglobin 550nm are compared to.
For stability studies of hemoglobin using this method, you must use only fresh gemolizat. When you do this, you need to consider, What haemoglobin concentration should be substantially 100 g / l.
Currently, for the identification of unstable hemoglobin β handling-merkuribenzoatom or β-chloromercuribenzoate with subsequent electrophoresis in gel krahmal'nom.
IN 1981 g. as the express-method proposed a new method of determination of unstable hemoglobin, based on the, that in the presence of zinc salts with low concentrations of unstable hemoglobin precipitates in temperature 37 ° C through 15 min unlike normal hemoglobin. While gemolizat in quantity 0,2 ml (6,21 mmol / l, or 100 g/l hemoglobin) Add to solution, contains 0,35 ml 0,003 M solution of zinc acetate and 1,45 ml 0,1 M TRIS-buffer pH 7,4. After mixing tubes are placed in the thermostat on 30 minutes at 37 ° C. In the presence of unstable hemoglobin appears residue, which settles through 30 m.
When some gemoglobinopatijah after pre-incubation of blood within 1-2 days, and sometimes in fresh blood metgemoglobina promoted.
On electrophoretic mobility (When researching on paper or acetatcelljuloze) of hemoglobin A is different, only one third of the known unstable haemoglobins. In some cases unable to identify modified electrophoretic mobility on krahmal'nom or polakrilamidnom gel. A study of the primary structure of unstable hemoglobin accurately set the type.
