Vascular-platelet hemostasis – The system of hemostasis
Endothelium, lining the inner surface of blood vessels, It is highly thromboresistant and plays an important role in maintaining the liquid state circulating blood. This property endothelium associated with the following features:
- the ability to produce and secrete into the blood potent inhibitor of platelet aggregation - prostacyclin (arachidonic acid metabolite, relating to prostaglandins);
- production of tissue activator of fibrinolysis;
- inability to contact activation of blood coagulation system;
- the creation of the anticoagulant potential at the blood / tissue by fixation on the endothelium of the complex heparin - antithrombin III;
- ability to remove from the blood activated clotting factors.
However, the walls of blood vessels due to their anatomical and physiological characteristics - stiffness, elasticity, plasticity and others - able to withstand not only the blood pressure, but mild traumatic external influences, whereby they prevent the occurrence of hemorrhage. This property, as well as the ability to withstand the output of red blood cells from the capillaries by diapedesis, t. it is. by mechanically intact vascular wall, usefulness depends on the characteristics of the endothelium and subendothelial layer structure - the degree of development and quality of collagen and microfibrils, the ratio of collagen and elastic fibers, basement membrane structure, etc.. d. These properties are highly dependent on the quantity and quality characteristics of platelets, whereby in low concentrations in blood and (or) thrombocytopathy amplified when both diapedetic bleeding, and brittleness microvessel: easily arise petechiae and bruising, become positive samples for capillary fragility - Pinch, cuff, Jar of A. AND. Nesterov, etc..
Microvessels respond to severe damage to local spasm - reflex and associated with the release of the vessel walls, and platelets epinephrine, noradrenaline, serotonin and other biologically active substances.
Damage to the walls of blood vessels and, in particular, exposure of subendothelial contribute to the activation of blood coagulation and platelet hemostasis in several ways:
- the release into the blood tissue thromboplastin (factor III, apoprotein C) and other activators of coagulation and platelet aggregation - adrenaline, noradrenaline, ADF and others.;
- contact activation by collagen and other components like platelets subendothelial (adgeziya), and blood coagulation (factor XII activation);
- production of plasma cofactor platelet adhesion and aggregation - von Willebrand factor, etc..
Thus, walls of blood vessels is closely related and interacts with all the other hemostasis, especially platelets.
Involvement of platelets in haemostasis It determined mainly by following their functions:
- angiotroficheskoy - The ability to maintain normal structure and function of microvessels, their resistance to damaging effects, impermeability in relation to the erythrocytes;
- the ability to maintain a spasm of blood vessels damaged by secreting (release reaction) vasoactive substances - Adrenaline, noradrenaline, serotonin and others.;
- the ability to plug the damaged vessels through the formation of a primary platelet plug (thrombus), including adhesion of platelets to subendothelium (adhesive function), bonding them to each other and clumping of swollen platelets (aggregation function), and synthesis, accumulation of secretion and activation of substances, stimulate the adhesion and aggregation;
- tromboplasticheskoy - The ability of platelets to allocate hemostatic factors.
All of the data is allowed to justify the doctrine of the unity of the vascular-platelet, or primary, hemostasis. The reason for this was the classical teachings Duke study, which showed, that the bleeding time under the skin of the ear lobe puncture needle or lancet (sample Dyyuka) increases regularly with severe thrombocytopenia, but it remains normal or almost normal in deep bleeding disorders (eg, Hemophilia). This data, Get full confirmation in further studies, led to the conclusion, that the primary hemostasis in microvessels is mainly due to platelet. This marked increase in bleeding time is recorded not only with significant thrombocytopenia (T in less than 30-50 1 l), but in severe forms of qualitative inferiority of platelets (Glanzmann thrombasthenia, trombocytopathies), as well as dysfunction of the cells of the secondary origin - because of the shortage of plasma cofactors adhesion and aggregation in the plasma or the presence of inhibitors of these functions (paraprotein, proteolysis products and others.).
Among the inherited forms of secondary platelet dysfunction most important and common in clinical practice is angiogemofilija (von Willebrand disease), in which the bleeding time is increased to 0.5-1 h and more, but from acquired forms - platelet dysfunction with disseminated intravascular coagulation (thrombocytopathy consumption, the damaging effect of proteolysis products), uremia, taking drugs (aspirin, antykoahulyantы, fibrinolytics et al.).
The formation of platelet plug and stopping the bleeding from microvessels completed during the sample for 2-4 minutes Duke, and to create an additional venous stasis (the imposition of a pressure cuff 5,3 kPa, or 40 mm Hg. Art., and more) - For 6-10 min.
Leading the primary hemostasis belongs adhesively-aggregation of platelets (AAFT).
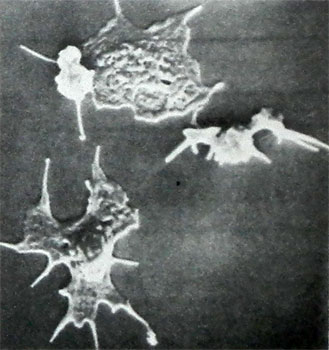
At present, we have been well studied basic mechanisms AAFT, develop affordable laboratory and instrumental methods of its investigation. Most often, the starter role in this process is the damage the walls of blood vessels, whereby the platelets come into contact with the subendothelial, in particular - the main stimulator of collagen adhesion, swell, forming processes and glued (adhere) at these sites.

The major plasma cofactors this process are calcium ions and protein-synthesized in the endotheliumvon Willebrand factor (factor VIII: RKOF) and platelets - which interacts with von Willebrand factor membrannыy glycoprotein Iin (SE-Iin).
In connection with this deficiency of vWF (angiogemofilija, or von Willebrand's disease) or GP-Iv (trombotsitodistrofiya, or Bernard-Soulier disease) accompanied by a sharp violation of platelet adhesiveness.
Along with the adhesion occurs platelet aggregation - Swelling and bonding them together to form shoots and superimposed units on land vascular injury, whereby the hemostatic plug or thrombus growing rapidly.
The primary incentive to produce collagen aggregation, released from the damaged vessel walls, and even more ADP from hemolyzed erythrocytes in the area of damage, kateholaminы and serotonin (L. 3. Barkagan, B. F. Arkhipov, 1980, 1983).
Platelet, suffer from adhesion and aggregation, actively secreted granules, which contain substances, reinforcing the process of aggregation and form its second wave. These include nonproteinaceous granules high electron optical density, containing a large amount of ADP, adrenaline, noradrenaline and serotonin, and α-granules, containing proteins - factor antigeparinovy (factor 4), b-тромбоглобулин, platelet-derived growth factor (mitogenic factor) and etc.
Later secreted granules, containing lysosomal enzymes (reaction liberation II).
The interaction between the platelet and plasma factors of hemostasis zone formed thrombin, small doses that dramatically enhance and complete the process of aggregation and also causes blood clotting, whereby the platelet-fibrin clot covered, becomes greater density, undergoes retraction.
An extremely important role in the regulation of platelet hemostasis play arachidonic acid, liberated from membrane phospholipids of platelets and vessel walls due to the activation of phospholipases.
Subsequently, under the influence of cyclooxygenase of arachidonic acid produced prostaglandins (PGG2, PGH2), and one platelet thromboxane produced under the influence of an extremely powerful aggregating agent - tromʙoksan A2 (TX2), and in the wall of blood vessels under the influence prostatsiklinsintetazy - the basic aggregation inhibitor - prostacyclin (prostaglandin I2, PGI2).
Violation education thromboxane A2 as a result of decrease in activity or blockade of cyclooxygenase or thromboxane leads to the expressed human platelets, promotes bleeding, which is observed in a number of hereditary and acquired (symptomatic) trombocitopatiй. Violation of the synthesis of prostacyclin in the vascular wall or a weakening of his admission into the bloodstream leads to an increased tendency of platelet aggregation, creates a risk of thrombogenic. The duration of action of the active thromboxane, prostacyclin and related prostaglandins small (A couple of minutes), but their significance in the regulation of hemostasis and pathology is very large. As a result of metabolism they become inactive derivatives - thromboxane B2 and other end products.
According to scientists, research that formed the basis of the doctrine of prostaglandin regulating platelet hemostasis, This mechanism is a trigger in the development of adhesive and aggregation of platelets. Activation of the platelet membranes may be not only the ADP and thromboxane, and hydroperoxides of polyunsaturated fatty acids, formed during the free radical auto-oxidation of phospholipids.
In addition to the above agents, in platelets and other blood cells activated (leukocytes etc.) are formed and other powerful stimulants aggregation. In recent years, particular attention is paid to fosfolipidnomu implemented plastinochnomu factor (PAF) of leukocytes and platelets, a 1-0-oktadecil-2-acetyl-3-fosforilholinom, as well as contained in α- granules of platelets glucoprotein G (thrombospondin, endogenous lectin). This factor is released from the platelets together with α-granules, fixed on the surface of activated blood platelets, forming a complex with nine fibrinoguenom, and in this form is used to implement trombinagregacii. For this reason, when trombocitopatijah lack of α-granules (eg, Gray platelet syndrome) disturbed aggregation of these cells influenced by Thrombin.
For the implementation of the platelet-platelet function adhesive needs a number of plasma cofactors aggregation — calcium and magnesium ions, fibrinogen, albumin and two protein cofactor, called agreksonami (A) and (B), Phospholipid cofactor, etc.
However, paraproteins, krioglobuliny and fibrinolnza products inhibit platelet aggregation. To protein inhibitors of this process include prostacyclin – dependent macromolecular protein, factor Barnes as Liana (decreases sharply when tromboticheskoj trombocitopenicheskoj purple) and etc.
In the implementation of the function of the platelet membrane glycoproteins play an important role of platelets, interact with agregirujushhimi agents.
According to the recommendations of the International Committee on Thrombosis and gemostazu, There are the following main types of membrane glycoproteins:
Glycoprotein I, consisting of two subunits — Ia and Ib. The first of these is von Willebrand factor and receptor is necessary for adhesion, and the second for Thrombin-aggregation. The contents of the glycoprotein I reduced under one of the variant forms of angiogemofilii and at trombocitodistrofija (Bernard-Soulier disease).
Glycoprotein II, also consisting of two subunits, required for all types of aggregation, the contents of his (especially IIb) dramatically reduced under trombocitoastenii Glanzmann.
Glycoprotein III, some of the components which connects with the glycoproteins IIb and calcium, is required for most types of aggregation and clot retraction; the contents of his reduced under trombocitoastenii Glanzmann
Functional value (IV) and (V) of membrane glycoproteins needs clarification.