Pancreatitis – Chronic pancreatitis – Acute pancreatitis
Description pancreatitis
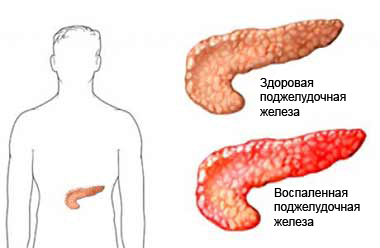
Pancreatitis – disease, in which the pancreas becomes inflamed. The pancreas is a long, oblate, pear-shaped organ, located on the bottom of the stomach. It produces digestive enzymes and hormones, including insulin. If pancreatitis producing digestive enzymes destroy their tissues.
Acute pancreatitis – It occurs suddenly, accompanied by severe pain in the upper abdomen (This form, if untreated, It can be life-threatening);
Chronic pancreatitis – progressive disease, which may destroy the pancreas.
Causes of pancreatitis
Causes of pancreatitis may include the following:
- Alcohol abuse (the most common cause);
- Gallstones and other obstructions in the bile ducts;
- Surgery or trauma of the pancreas;
- Taking certain medications;
- Unknown causes (about 15 % cases);
- Elevated blood triglyceride levels (hypertriglyceridemia);
- Infection (Bacterial, Viral, Fungus, or parasitic);
- HIV infection;
- Congenital pancreatic;
- Complications of ERCP (endoscopic retrograde cholangiopancreatography).
Risk factors
Factors, which increase the risk of pancreatitis:
- Alcohol abuse;
- Heredity;
- Short bouts of acute pancreatitis;
- Medication, including:
- Estrogens;
- Sulfonamides;
- Tetracikliny;
- Tiazidы;
- Pancreatic cancer;
- Hyperlipidemia (high levels of blood fats);
- Hypercalcemia (elevated blood calcium);
- Viral infections, such as mumps.
Symptoms of pancreatitis
Symptoms include:
- Severe pain in the center of the upper abdomen, that:
- Sometimes it extends in the upper back;
- Often increases with food, walking, or lying on the back;
There are less severe symptoms in chronic pancreatitis, a gradual increase:
- Nausea and vomiting;
- Diarrhea;
- Temperature;
- Jaundice (yellowing of the skin);
- Shock change in the vital processes of the body (eg, fast, but weak pulse, rapid and shallow breathing, and low blood pressure in cases of severe);
- Unexplained weight loss;
- Symptoms of Diabetes:
- Increased thirst;
- Increased urination;
- Fatigue.
Diagnosis of pancreatitis
On examination, the doctor may ask about the frequency and amount of alcohol consumption, as well as various drugs. Other tests may include:
- Blood tests, to measure levels of certain digestive enzymes and check for biliary obstruction and complications of pancreatitis (eg, diabetes, renal failure, infection);
- Abdominal ultrasound or abdominal CT scan – Search for gallstones and determine the extent of pancreatic inflammation;
- Magnetic resonance cholangiopancreatography (MRHPG) – analogue MRT, in which examined the pancreas, pankreaticheskiй flow, and nearby bile ducts;
- Endoscopic retrograde cholangiopancreatography (ERKhPG) – using a special camera, introduced through the mouth into the pancreatic duct studied the negative effects of pancreatitis and diagnosis of diseases, associated with the pancreas and bile ducts.
Treatment of pancreatitis
Acute pancreatitis
Treatment for acute pancreatitis depends on the severity of the attack. Sometimes it may be necessary hospitalization. The main goal of treatment is, to rest the pancreas. In some cases this means fasting for 3 – 4 days. In severe cases, the patient can not take food for 3 – 6 weeks. Maybe this time it will be necessary to take strong painkillers.
Treatment may also include:
- Intravenous drug;
- Intravenous administration of nutrients, if the patient is unable to eat for a long period of time;
- Antibiotics, the presence of infection.
Chronic pancreatitis
The goal of treatment of chronic pancreatitis consists in, to relieve pain and treat nutritional and metabolic problems. Specific steps include:
- Strict prevention of alcohol;
- Less fatty foods;
- The adoption of tablets, containing pancreatic enzymes, to aid with the digestion of food;
- Injections of insulin, to change the level of sugar in the blood (If diabetes develops );
- Frequent eating small portions.
Surgery and/or ERCP may be necessary in cases:
- Opening a blocked pancreatic or bile duct;
- Removing parts (or rarely entire) pancreas;
- Drainage of pancreatic cyst.
If the diagnosis of pancreatitis, You should follow the instructions of your doctor.
Prevention of pancreatitis
The best way to avoid pancreatitis – limit alcohol consumption. If the patient is Hyperlipidemia, you want to limit your intake of fat and follow the advice of a doctor, to lower lipids.
