The definition of quantitative and qualitative characteristics of sperm
Determination of sperm motility
Determination of sperm motility is an important parameter, of the quality of the ejaculate. Sperm, capable of fertilization, have mobility - Make straight forward motion at the speed of 50 m / s. Can be found in the ejaculate sperm with impaired mobility - diskinospermiey in the form of vibrational, Manege and other movements, which normally are absent.
Sperm motility was evaluated in native preparation of ejaculate with a limited field of view (using window Fonio), Using the eyepiece lens 7X and 40X, when hooded condenser. Counting 100 cell, note the number of them moving, sedentary and fixed sperm. Normally, active-motile sperm are 80-90 %, sedentary - 10-12, fixed - 6 10 %. Taking into account only those active-moving and slow-moving sperm, who make steady progress.
You can also use a more detailed five-point rating scale:
- "4" - great mobility (all have a rectilinear translational sperm motility at a significant rate);
- "3" - good mobility (a few drops);
- "2" - mediocre mobility (Still a lot of sperm, but with vibrating tail);
- "1" - poor mobility (the lack of forward movement, Only the tail of sperm motility);
- "0" - the movement of sperm missing.
Fertility ejaculate It depends on the duration of sperm motility, therefore it is necessary to determine sperm motility in dynamics (Dynamic kinezisgramma).
A drop of semen is applied to the cover glass, turn it upside down and put on a glass slide with a crescent for the hanging drop so, the drop was in the center of the recess. The edges of the coverslip lubricated with liquid paraffin and microscopically determining the percentage of actively motile-, sedentary and fixed sperm through 1, 3, 6, 12 and 24 hours after ejaculation. Research is conducted at room temperature. Normally, the number of active-motile sperm decreases every 2-3 h 20 % ,
- Note. Microscopic examination of semen must be carried out in the laboratory of one person, have sufficient experience in the field of laboratory diagnostics, as the results of the determination of sperm motility in different researchers range up to ± 40 % and depends largely on the experience with the ejaculate.
The trial on the "revival" of sperm
The trial on the "revival" of sperm It based on the restoration of normal mobility of fixed, but live sperm by means of stimulating solutions:
1) Becker solution (Glucose - 3 g, On2HPO4 - 0,6 g, NaCl — 0,2 g, KH2AFTER4 -0.01 G, distillirovannaya to water 100 ml; pH — 7,8);
2) 0,1 % caffeine solution (not only in ampules!) - 10 % the volume of ejaculate;
3) 0,1 M arginine solution.
Method. Dimensional pipetter 1 ml nasasyvayut 0,1 ml of ejaculate (well mixed) and the same pipette gaining 0,9 ml solution stimulating. The content of the pipette is blown on a watch glass, mix well by repeated suction and blowing fluid on a watchglass, and then the finished product hanging drop. Through 5 10 min fixed, but live sperm begin to move.
The percentage of motile sperm determined immediately when restoring mobility and after 3, 6, 12 and 24 no. For more reliable results, is carried out parallel to the sample with two challenging solutions. Only if it is impossible to "revive" the sperm can still talk about nekrospermii.
Identification of live sperm among fixed
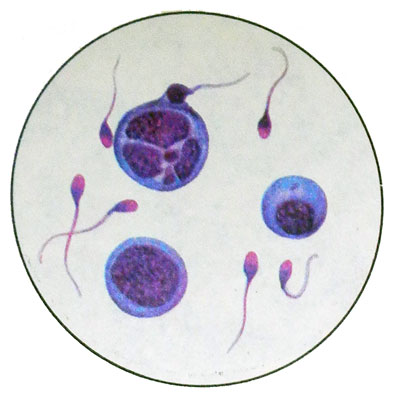
The principle of the method is based on the, enzymes that live sperm decolorized eosin. As reagents are used 5 % aqueous solution of potassium and eosin 10 % aqueous Nigrosine.
Method. On slide cause a small drop of semen, placed near twice the drop 5 % eosin solution and a drop of potassium 10 % Nigrosine solution, is also twice as large drops eosin potassium. First, the ejaculate is mixed with potassium eosin, waiting a few seconds, and then mixed with a drop of Nigrosine, again waiting a few seconds and make thin smears polished glass slide.
Using an immersion system microscope, in the smears are counted at least 200 sperm, highlighting living (Colorless) and the dead (eosin stained red). The number of live and dead spermatozoa expressed as a percentage. In the absence of Nigrosine drop semen mixed with straw 5 % eosin solution of potassium and prepare thin smears for microscopy. Nigrosine dyes only the background of the drug, where sperm are allocated more contrast. Normally live sperm 80-90 % of the total number.
Counting the sperm in 1 ml, and in the entire volume of ejaculate
The number of sperm in 1 ml throughout the ejaculate are calculated in a counting chamber Goryaeva.
The number of spermatozoa in the entire ejaculate is determined by multiplying the number of sperm in 1 ml amount of ejaculate (milliliters).
- Note. The counting chamber can also determine the number of motile sperm, Why ejaculate should be diluted with warm isotonic sodium hloridz and count the number of fixed sperm, and then subtract it from the total.
Normally, in the 1 ml of semen contains 60-120 million. sperm, when giperspermii - more 120 million., in oligo - from 30 to 60 million., what, usually, making it impossible to fertilization. However, the described cases, When fertilization occurs and Content 1 ml of эyakulyata 5 to 30 million. sperm.
Anyway in identifying oligospermia 2-3 necessary controls counting the number of sperm with intervals of 3-4 weeks to determine their maximum amount. At the same man's sperm count is subject to considerable fluctuations in physiological.
Normally around the ejaculate contains more than 150 million. sperm.
Counting spermiogram
Spermiogram - is the percentage of the different morphological forms of sperm cells and spermatogenesis.
In a smear, stained with hematoxylin-eosin or Pappenheim, calculated minimum 200 sperm, wherein the number of normal and pathological forms, and spermatogenic cells expressed in percentage. Calculation is made using the immersion microscope systems and machines for counting leukogram pre altered the names of keys.
In a normal ejaculate sperm normal forms is 80-85 %, sometimes 100 %, these include physiological variations, characterized by unusual or neck, or reduced, or enlarged head.
Young, or immature, shaped sperm have around the head and neck of the rest of the cytoplasm ("Collar"), observed with frequent sexual intercourse and are not capable of fertilization.
The old forms of sperm (hyperchromia, axromija, vacuolation head) appear in the ejaculate after extended abstinence and not suitable for fertilization.
Pathological forms include sperm with deformities of the head: megalospermatozoidы (gigantospermatozoidы), macro-, mikrospermatozoidy, Conical, two headed sperm with a neck and a tail, without neck with one or more tails, without a tail, without the tail head, etc..

In healthy men in a normal ejaculate abnormal sperm forms are usually not found, but sometimes their number during normal fertility can reach the ejaculate 20 %, of which approximately 15 % head of the pathology, 3-5 % - Body, 2-5 % - Tail.
In pathological spermatogenesis, secretory form of infertility identified sperm with abnormal head and neck. Pathology tail usually excretory origin, It occurs during the passage of sperm vas ways.
In stained preparations are also clearly visible separately located germinal cells at various stages of differentiation and maturation, it is important to differentiate aspermia and azoospermia.
Spermatogonia are rounded, sometimes oval, diameter of 5-12 microns. The core occupies about a third of the cells, dark- or light colored, 1-2-3 Nucleo- Lama, often located near karyotheca (nuclear envelope), chromatin structure melkozernystaya. The cytoplasm is narrow, basophilic, Homogeneous. Spermatogonia divide mitotically several times. There are cells with well-defined stages of mitosis.
Some of the cells, formed through mitosis, differentiated into spermatocytes I, and then II order. Spermatocyte I order - Round or polygonal cells with a diameter of 17-19 mm with a large round nucleus and cytoplasm light fine. In stained preparations is a clear perinuclear zone.
Spermatocytes II of the order formed as a result of meiosis. They are smaller, than spermatocytes I order (diameter 15 m), but in morphology almost identical. In the ejaculate more common, than spermatocytes I order, but much less frequently, than spermatids.
Spermatydы - Small, round or elongated cells with a diameter of 12-15 mm with round hyperchromatic nuclei, located centrally or eccentrically. There may be a multicore spermatids. Pale cytoplasm, bazafilnaya, often vacuolated.
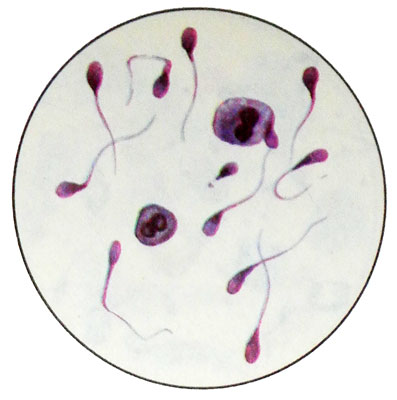
Spermatids are transformed into spermatozoa.
The cells of spermatogenesis in normal spermiogram is not more than 2 %. A large number of infertility observed in the secretory nature.
For phase contrast microscopy ejaculate is diluted with isotonic sodium chloride solution with the addition of a small amount 1 % aqueous solution rivanola or carbolic acid to reduce sperm motility.
With fluorescent microscopy It is applied onto a glass slide and a drop of ejaculate a drop of acridine orange in the breeding 1:20000. The drops are mixed and covered with a cover glass. Microscope eyepiece used 7X and 40X objective. Live sperm are stained green, dead - orange. Normal and abnormal sperm forms are easy to distinguish because of their morphological features.
Rabotы rules of phase-kontrastnom and lyuminestsentnom microscope opisanы in instruktsiyah k эtim Instruments. When using phase-contrast and fluorescence microscopy spermiogram calculated by the general rules.
On the basis of a microscopic examination of the ejaculate can identify various pathological conditions.
- Spermatoschesis - The absence of sperm in the ejaculate, and the cells of spermatogenesis.
- Azoospermia - Absence of sperm cells in the presence of spermatogenesis.
- Asthenospermia - Decrease in the number of motile cells and an increase in the number of pathological forms under normal total number of sperm.
- Oligoastenospermiya - Reducing the number of sperm and their mobile forms and increasing the number of pathological forms.
- Nekrospermiya - Fixed all the sperm in the preparation even after the "revival".
- Akinospermiya - State, in which, in contrast to the previously fixed nekrospermii sperm after the "revival" are beginning to move.
