Coagulation hemostasis – The system of hemostasis
Blood clotting - a complex enzymatic process, which involved a number of proteolytic enzymes, and non-enzymatic protein and phospholipid components, dramatically accelerating and strengthening the activation and the action of enzymes.
Conventionally, blood coagulation process can be divided into two main phases:
- initial multi-, leading to activation of prothrombin (factor II) to convert it into an active enzyme - thrombin (IIa);
- final, wherein under the influence of thrombin, fibrinogen is converted first into fibrin monomers and dimers, and zatem - in fibrin polymer, which is stabilized activated Factor XIII.
According to the international nomenclature, All clotting factors, Besides – platelet, designated by Roman numerals (in the table).
Characteristics of blood clotting factors | |||||
Digital signage | The most accepted names | Plasma levels, g / l | Activity, % | The half-life in blood plasma after intravenous administration | Minimum, necessary for hemostasis |
| I | Fibrinogen | 1.8-4.0 | – | 3-5 Days | 0,8 g / l |
| II | Prothrombin | To 0,1 | 80-120 | 3-4 Days | 40% |
| III | Tissue thromboplastin | 0 | 0 | ? | – |
| IV | Calcium ions | 0,9-1.2 Mmol / l | – | – | – |
| V | Ac-globulin (proakcelerin) | To 0,01 | 70-150 | 18-24 | 10-15% |
| VII | Prokonvertyn | " 0,005 | 80-120 | 4-6 | 5-10% |
| VIII | Antigemofilьnый globulin (AGG)
| 0,01-0.02 | 60-250 | 12-18 | 30-35% |
| IX | PTC factor (Plasma Thromboplastin component), Christmas factor | To 0,003 | 70-130 | 20-30 | 20-30% |
| X | Factor Stuart-Prauera | " 0,01 | 80-120 | 48-56 | 10-20% |
| XI | PTA factor (Plasma Thromboplastin antecedent), plasma thromboplastin predecessor | " 0,005 | 70-130 | 60 no | ? |
| XII | Hageman Factor, contact factor | To 0,03 | 70-150 | 2-3 Days | less 1 % |
| XIII | Fibrinstabiliziruyuschy factor (fiʙrinaza) | 0,01-0,02 | 70-130 | 2-3 Days | 2-5% |
| Plasma prekallikrein, Fletcher factor | To 0,05 | 60-150 | ? | less 1 % | |
| High molecular weight kininogen (WMC), Fitzgerald factor, Factor Flodzheka, Factor Williams | To 0,06 | 80-130 | ? | less 1 % | |
To indicate, These factors were subjected to activation, numeric character factor is added the letter «a», and in the case; if the active principle active factor becomes one of its fragments,— letter «f»
In addition to digital signage, and other names are used coagulation factors - according to their function (eg, Factor VIII - antigemofilьnый globulin), by the names of patients with newly: discovered deficiency of a factor (factor XII - Hageman factor, Factor X - Factor Stuart-Prauera and etc.), at least - by author name (eg, von Willebrand factor).
Counteract blood clotting primary (independently synthesized) and secondary, formed during coagulation and fibrinolysis physiological anticoagulants.
Fibrinogen into fibrin transformation
Consideration of the clotting advisable to start with its final stage, lies in the fact, that the proteolytic enzyme Thrombin, resulting from its inactive precursor - prothrombin, cleaved from the fibrinogen molecule four peptides (two peptides A and B two peptide), resulting in the formation of fibrin monomers, each of which has four free connection. By connecting these connections monomers with each other, first in pairs - in dimers, and then - in polymers (compounds of the type of "end-to-end" and "side to side"). Fibrin fibers are formed.
Fibrinogen - globulyarnыy glycoprotein (molecular weight 340000), consisting of two identical subunits. Each subunit is composed of three chains - Aα, Bv и c.
Thrombin cleaves the beginning of this molecule peptides A (forming a des-A-fibrin monomers), then - B peptides (des-AB or full fibrin monomers). The appearance of free peptide A in the blood circulation (determined immunologically using anti-A-serum) a sign thrombinemia and used as a "witness" intravascular coagulation (at DIC, massive thrombosis).
Fibrin monomer have trehnodulyarnuyu structure, and compound the polymer flows steps of forming dimers, of which the longitudinal and cross-linking are formed protofibrils, and then - the fibrin fibers. This soluble fibrin 5-7 M . urea or 2 % monochloroacetic acid, in connection with what he referred to as fibrin S (soluble). Under the influence of factor XIII, which is also activated by thrombin in presence of calcium ions, in fibrin formation as an additional disulfide bonds between γ-, and the α-chain, making it. nerastvorimыm in fibrin I mochevine- (insoluble).
Under normal conditions, has relatively moderate concentrations of thrombin (eg, causing coagulation of blood plasma from 10-12) provide complete transformation of fibrinogen to fibrin, whereby in this serum protein and other immunological methods have not determined.
In contrast,, in processes, characterized by intravascular coagulation, reduced sensitivity to thrombin and to some extent impaired fibrin polymerization process monomers, whereby thrombin clotting time is lengthened and the above threshold doses of thrombin is not coagulated whole fibrinogen. Violation of this is due to the fact, that part of complete and incomplete fibrin monomers form complexes with fibrinogen and, probably, with early cleavage products of fibrin and fibrinogen by plasmin. These macromolecular and MIDDLE soluble fibrin monomer complexes (RFMK), referred to in the literature as well as the "bad coagulant fibrin", "Blocked fibrinogen", bad coagulated under the influence of thrombin (are relatively resistant thrombin-), but form a gel when added to plasma 50 % ethanol (ethanol test), Some samples protamine sulphate, solution of β-naphthol in 50 % alcohol, sour ortofenantrolina.
The phenomenon of non-enzymatic coagulation SFMC (Locked fibrinogen) called phenomenon paracoagulation and it is widely used in laboratory diagnostics and thrombinemia intravascular coagulation. The most fully identify these complexes allows the following tests:
- coagulation test with Central Asian snake venom ephah;
- sample ortofenantrolinom;
- Test adhesion of staphylococci.
Thus, transformation of fibrinogen to fibrin can go both conventional manner, and forming SFMC (Product paracoagulation), the identification of which is essential for the diagnosis of intravascular coagulation.
Overall assessment of the final stage of the process of coagulation It is carried out by thrombin test, t. it is. by determining the clotting time of citrated plasma by adding to it a standard amount of thrombin. The test is important for diagnosis of many disorders of blood clotting, the results are important for the correct interpretation of the testimony of all the other coagulation samples, For the inhibition of the final stage of the process lengthens the clotting time in all the other studies,.
Mechanisms of prothrombin to thrombin
According to the modern theory of the complex cascade-clotting, activated prothrombin (factor II) It is the result of multi-enzyme process, wherein successively activated and interact various coagulation factors. Of these factors III, VII, X, IX, XII and XI, and prekallikrein are proteolytic enzymes, and factor VIII, V - non-enzymatic process aktseleratorami, accelerating the activation of enzymatic factors many thousands of times.
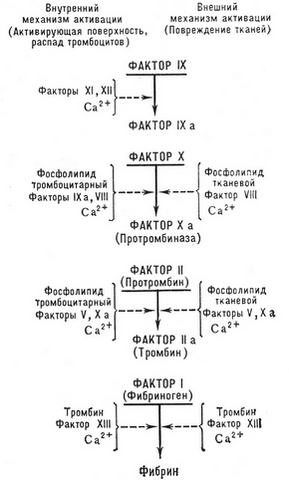
There are two main mechanisms start the clotting process - external and internal.
Outside the mechanism of blood clotting
Outside the mechanism of blood clotting triggered by tissue thromboplastin, which may enter the blood plasma of the affected (injury, surgery and other.) tissues, vessel walls (It is produced by endothelial damage, with the participation of activated platelets), and enter the bloodstream from the tissue fluid (amniotic fluid embolism, peritoneal-venous shunting, Various types of shock). Directly in the blood tissue thromboplastin may be produced by activated monocytes (under the influence of endotoxin, immune complexes, etc.. d.).
In a large number of tissue thromboplastin produced by cells and certain cancers (including leukemia).
The current starting tissue thromboplastin is a protein - apoprotein C, whereas the phospholipid part III nonspecific factor and serves as a process of activating matrix (t. it is. functionally similar to the factor 3 Platelet, kefalin, eritrofosfatidom).
From circuit clotting seen, Tissue thromboplastin that forms a complex with calcium ions and Factor VII, activates the last, resulting in a potent activator of the enzyme Factor X.
In the laboratory test simulates an external mechanism of prothrombin time, in the performance of which to recalcified citrate plasma is added to the outside fabric (most of the human or rabbit brain) thromboplastin specific activity and the clotting time recorded.
The internal mechanism of blood clotting
The internal mechanism is much more complex and important for deciphering the pathogenesis and diagnosis of the most frequently encountered in clinical practice, hemorrhagic diathesis - hemophilia A and B, angiogemofilii, or von Willebrand's disease (they accounted for more 97 % all hereditary hemorrhagic coagulopathy).
When an internal blood clotting mechanisms (plasma) implemented without the participation of tissue thromboplastin.
Triggering factor of this mechanism is the factor XII (Hageman), activation of which is due to contact with blood or foreign surface (glass, metal, kaolin, etc.. d.), either subendothelial (Collagen) and other connective tissue components, that observed when damaged blood vessel walls (mechanical injuries, vaskulit, atherosclerosis, etc.. d.).
Besides, Activation of factor XII may be performed by its enzymatic cleavage (kallikreinom, plasmin or other proteases). Hence, There are two kinds of activation of factor XII:
- and) pin - to form Factor XIIa;
- to) Enzyme - to form the active factor XII fragments (XIII).
There are some quality differences between the effect of factors XIIa (largely affects the clotting) и XIII (It has a greater activating effect on the kallikrein-kinin system and fibrinolysis). In general, factor XII is a universal activator of plasma proteolytic systems - coagulation, kallikrein-kinin, fibrinoliticheskoy and complement sistemы.
In the initial (contact) phase of the coagulation process takes place, one side, Mutual activation of factor XIIa and kallikrein in the complex factor XII - prekallekrein - high molecular weight kininogen, and then - the activation of factor XI in a complex of factors XIIa - XI - WMC.
This initial phase of the longest (4/5 all clotting time), activated with the growth area and the duration of the contact of blood with a foreign surface (minimal activation in silikonirovanii utensils and more rapid the study after taking blood from a vein, maximum - at dobavlenyy kaolyna). It is important to take into account, activation of the contact factors XII and XI occur in the stabilized oxalate or citrate blood plasma, t. it is. It does not require calcium ions. Participation of calcium in blood clotting begins only after activation of factor IX, t. it is. Education next set 2.
When you create a maximum contact with kaolin and sufficient factor 3 platelets or kephaline (t. it is. in the activated partial thromboplastin test) attenuation factor XI activation and deceleration can be caused by clotting factor deficiencies XII, XI. prekallikreina, high molecular weight kininogen (WMC). The most common deficiency of factor XI, others disorders are very rare.
More often violation of the internal mechanism of clotting associated with a defect of the next phase - activation of factors IX and VIII. Usually, this is due to a deficiency of factor VIII Component, t. it is. with hemophilia A and von Willebrand's disease or angiohemophilia (about 93 % All patients), less often - with Factor IX deficiency (hemophilia B).
Great value for the clinic factor VIII requires a more detailed review of data on its structure and functions.
According to current data, Factor VIII is a protein polymer, consisting of a number of identical subunits. In each of the subunits include the following components:
1) coagulation of the (VIII: FROM) and its antigen (VIII: Dog);
2) von Willebrand factor (FV) or cofactor ristomitsinovoy platelet aggregation (VIII: FV, VIII: PKOF) antigen and (VIII: Cardiovascular, VIII: Cardiovascular / FV);
3) carbohydrate portion and, perhaps, another unidentified protein component.
Place synthesis VIII:FROM not determined, This is controlled by gene synthesis, located on the X chromosome; isolated violation of its characteristic of hemophilia A.
Synthesis of von Willebrand factor (FV) controlled by autosomal occurs almost exclusively in the endothelium, whereby the factor is used as a marker of endothelial; its blood level rapidly increases when many vascular diseases.
Deficiency of von Willebrand factor or a change in its multimeric structure is a violation of the vascular-platelet hemostasis (prolonged bleeding, violation of platelet adhesion to glass and collagen or ristomycin-platelet aggregation), and decrease the activity of coagulation VIII:FROM. These disorders occur in different combinations in different variants angiohemophilia. The blood contains both vWF in plasma, and platelets (в a-гранулах), and within these cells, he dissociated from VIII:FROM. In hemophilia A level VIII:With the sharply reduced, while the content in the plasma VIII:EF remains normal.
Factor VIII:FROM - Nefermentnый accelerator factor IXa, with which it forms a complex on the phospholipid matrix. Activated VIII:With the feedback-low doses of thrombin (IIa) and, perhaps, Factor Xa; thus it dissociates with EF. Following the activation of thrombin cleaves and inactivates factor VIII:With both directly, and indirectly through activation of protein C.
The interaction of external and internal mechanism of blood clotting
In the body of the external and internal mechanisms of activation of blood coagulation system is not divided, and intimately interact with each other. So, Factor XII + kallikrein activate factor VII. An important role is also played by mutual activation of factor VIIa and IXa, and Xa and VIIa.
Factor VIIa partially activated as plasma lipoproteins and triglycerides, and retrograde thrombin. For this reason, the identification of activating and enhancing factor VIIa is a global marker of intravascular activation of blood coagulation and high thrombogenic risk, especially coronary heart disease and hyperlipidemia.
As with external, and in the internal mechanism of coagulation interaction and activation of factors made on phospholipid mikromembranah, the template, which are fixed (via calcium ions), change their tertiary and quaternary structure, intensely react with each other protein factors. The role of the matrix performs the membrane platelet membranes and granules (factor 3 Platelet) , and similar components from other cell membranes (erythrocytes, etc..). To a large extent the presence of these membrane phospholipid matrix determines the, that, other things being equal between plasma coagulation, containing a small amount of platelets, longer, than the clotting time of plasma with normal platelet count, and then, what gemoliz (release of erythrocyte membranes) greatly accelerates clotting and distorts evidence coagulation tests (does hemolyzed blood unsuitable for studies of blood coagulation).
Due to varying conditions phospholipid activation indication non-standardized coagulation tests are subject to a very large random fluctuations. This spread is even increased because of unequal intensity (properties of glass tubes) and the duration of activation of the contact factor XII. The standardization of coagulation tests of contact (receipt and processing of blood under silikonirovaniya glassware or in PTFE tubes with subsequent activation of the maximum contact phase kaolin) and phospholipid activation (the addition of a standard amount of kephaline) It is making them much more accurate and reproducible.
To assessment of platelet clotting activity should be compared kaolin clotting time of plasma with high and low content of platelets (eliminating from the reaction cephalins).
Thus, a full assessment of the clotting process when you start it in the inner mechanism by means of general studies clotting time standardized tests - kaolin and kaolin-kefalinovym (activated partial thromboplastin time), and the two-stage test autokoagulyatsionnym.
Likewise activated and inactivated other non-enzymatic coagulation accelerator - Factor V, interaction with factor X. This complex is called in the literature protrombinazy (by outdated terminology - blood thromboplastin), in which the activity of the enzyme is often a factor Xa, transformiruyushtiy prothrombin to thrombin. In the phospholipid matrix (eg, on the platelet membrane) Activity in this complex 1000 times higher, than in the absence of phospholipid. The complex is in the Va-Xa 3000 times more active, than factor Xa. Thus, Factor Va and phospholipid matrix together elements increase the activity of prothrombin in comparison with isolated factor Xa in 300000 time.
On the surface of each platelet has about 3000 phospholipid receptor complex Va-Xa, of which about 1000 high-affinity receptors. Matrices for all complexes of clotting factors can serve as phospholipid micromembrane Kefalonia and erythrocyte membranes (éritrocitin, eritrofosfatid), that is widely used in laboratory practice.
When activating factor Xa prothrombin is converted into the active α-thrombin. Thus from it sequentially cleaved fragment 1 remains prethrombin 1, and then - a fragment 2 remains prethrombin 2. With such a single-stranded molecule of prothrombin cleavage transformed into double-stranded (cleaves A and B) молекулу a-тромбина. Then the latter subject autolyze and loses Activity, as well as the physiological inactivated antithrombin.
Under the influence of other endo- and exogenous (venoms of snakes and so on.) Proteolytic enzymes may be formed form thrombin, characterized by α-thrombin weaker coagulant activity, less sensitivity to complex heparin - antithrombin III and other properties.
Ionized calcium is essential for blood clotting, because it is involved in the following processes:
- molecular conformation of coagulation factors to the active form;
- fixing interacting factors in the phospholipid matrix;
- accelerating the activation of individual factors by joining them (eg, transformation of prothrombin to thrombin accelerates the Ca in 1000 just by connecting it to γ-karboksiglyutamilovym residues in NH2-terminal part of the molecule).
When analyzing the results of basic coagulation tests, it is important to consider the following:
- used in assay systems Factor VII participates only in the external mechanism of the process, whereby when it is extended only about deficit- thrombin time;
- Factor XII, XI, IX, VIII and prekallikrein participate in the internal mechanism of activation, and therefore when they are violated deficit aPTT and ACT, whereas the prothrombin time is normal;
- Factor X deficiency, V, II and I, which closes both the clotting mechanism, Pathology revealed in all the above tests.
However, the external and internal mechanisms of activation are not isolated from each other, interact with each other.
So, found mutual activation of factor VII and factor IX, and X, as well as the activation of factor VII complex XIIa-kallikrein-WMC. The inclusion of these "bridges" between internal and external mechanisms is one of the diagnostic criteria for the condition or latent prethrombotic intravascular coagulation. It is detected by an increase in activity of Factor VII in plasma during testing it on plasma, devoid of this factor, as well as through the test of cold activation of prothrombin time with bovine thromboplastin.
Many coagulation factors and fibrinolysis are synthesized in the liver. Of these factors II, VII, X and IX, and anticoagulants - proteins C and SK- vitaminozavisimy: the final step of their synthesis (carboxylation) violated the deficit phylloquinone (Vitamin K) and influenced by his antagonists - coumarin, fenilina etc.. This disrupted education in hepatocytes K-vitaminozavisimoy carboxylase, depriving coagulation factors ability to activate. Opisan naslyedstvyennyi gyemorragichyeskii diatyez, in which the result of violation of the synthesis of the carboxylase reduced level of K-vitaminozavisimyh clotting factors.
In contrast,, V factor and a number of components of the fibrinolytic and the kallikrein-kinin system are synthesized in the liver, regardless of phylloquinone.
