Axalazija – Esophageal achalasia
Description esophageal achalasia
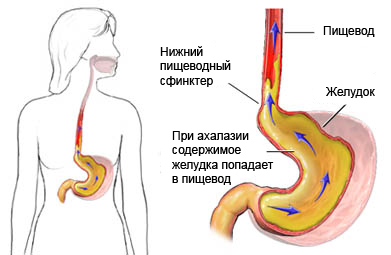
Achalasia is a relatively rare disorder of the smooth muscle of the esophagus. The esophagus is a muscular tube, through which food and fluid gets out of his mouth to the stomach. Achalasia makes it difficult ingress of food and liquid into the stomach through the esophagus.
Causes of esophageal achalasia
The body has a muscle, called the lower esophageal sphincter (NPC). It is located in a place, where the esophagus meets the stomach. If swallowing is not, LES remains closed, to prevent ingress of food, liquids, and gastric juice back into the esophagus. When swallowing nerves serving the muscles signal, and they push food down the esophagus (action, called peristalsis) and NPC opens.
In people with achalasia nerve endings in the esophagus and the lower esophageal sphincter do not work correctly. This leads to:
- The absence of peristaltic (muscle) activity;
- Failure to open up fully NPC.
Achalasia is associated with the low sensitivity of nerve cells in the esophagus, and the reason for this process is unknown.
Risk factors for esophageal achalasia
Because the exact cause of achalasia is unknown, Risk factors are unknown.
Symptoms of achalasia
Symptoms achalasia most common between the ages of 25 to 60 years. Symptoms rarely develop in children. Symptoms tend to be mild at first, and then get worse over months or years. Cardinal symptom – difficulty swallowing solid food, and, during progression disorders, liquids. From 70% to 97% patients with achalasia have difficulty swallowing solid foods and liquids.
Other symptoms may include:
- Discomfort or pain in the chest (under the breastbone, especially after eating);
- Cough, especially in the supine position;
- Heartburn;
- Weight loss (as a violation of progress);
- Vomiting. In some people, this symptom occurs during sleep. This can result in inhalation of food particles or liquid, which can lead to aspiration pneumonia and other respiratory infections.
Diagnostics
To diagnose achalasia need to pass the following tests:
- Manometrija – the tube is inserted into the throat to test the pressure in the esophagus and the stomach when swallowing;
- We need to do an x-ray of the esophagus – procedure is carried out after receiving barium salts (thick liquid, visible on x-ray).
- Endoscopy of the upper portions of the stomach (esophagoscopy) – the esophagus is seen directly through a fiber-optic tube to look for other causes of disease.
Treatment of achalasia
The goal of treatment is, to facilitate the opening of the NPC. Treatment may include:
Pneumatic expansion of the lower esophageal sphincter
This treatment stretches the LES muscle. A thin tube is inserted into the throat. At the end of the tube is uninflated balloon. Once the tube reaches the muscles NPC, the balloon is inflated. Pneumatic expanding fairly effective treatment for achalasia. It – the main treatment for most patients, although the procedure, perhaps, It should be repeated.
The use of botulinum toxin
A tiny amount of botulinum toxin, Type A, NAP is introduced into the. Botulinum causes the LES to relax, which facilitates the opening. Since the effect is temporary injections must be repeated.
Surgery
Small incisions are made in the NPS, to help him relax. This is called Heller myotomy surgery. This operation is usually performed through laparoscopy, and it is relatively simple. Because the NPS partially cut, about 15 % Patients experiencing symptoms of gastroesophageal reflux disease (Heartburn) after surgery.
Medication
In some cases, certain medications may help relieve symptoms temporarily. Preparations, that reduce LES pressure, include:
- Nifedipine;
- Nitroglycerin.
Prevention achalasia
Methods of prevention of achalasia no, because the cause of the disorder is unknown.
